Peripheral Vascular Disease
1. Peripheral vascular disease (PVD) or Peripheral arterial disease (PAD) - What does the term mean?
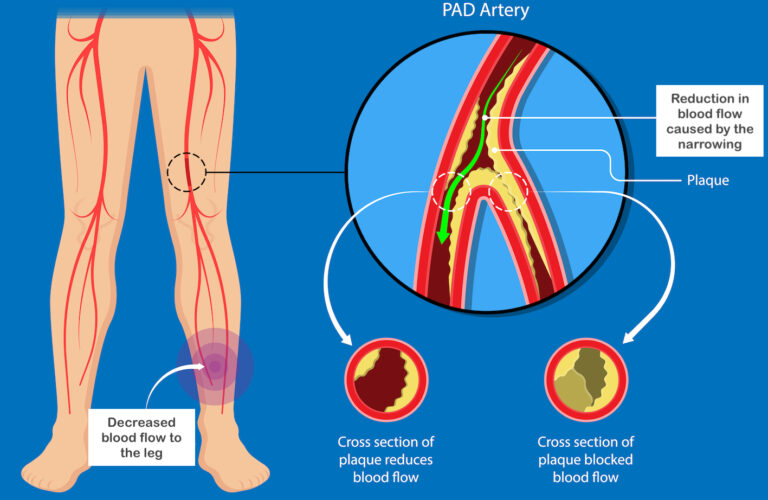
PVD or PAD refers to the narrowing or block in the blood vessels supplying the legs or the arms. The problem usually occurs in the blood vessels (arteries) of the legs.
The narrowing occurs due to a slow, progressive process called “Atherosclerosis”. In this process, there is deposition of a material called ‘Atherosclerotic plaque’ in the wall of the artery. This plaque is made of fat, cholesterol, calcium and other substances. The factors that contribute to the formation of the Atherosclerotic plaque are answered under Question No. 3
2. What are the symptoms of Peripheral vascular disease?

Pain, especially in the calf region, which develops during walking or exercise and subsides during rest is very characteristic of PAD. This is called ‘Claudication’ pain. Pain is worsened during walking or exercise as more blood (and Oxygen) is needed during these activities. As we take rest, the requirement for oxygen reduces and pain gradually subsides.
With worsening narrowing or blockage of arteries, the pain gradually worsens and starts manifesting even at rest (called ‘rest’ pain).
‘Claudication’ pain and ‘Rest’ pain are usually felt in the calf region, but may also be felt in the thigh or the buttocks.
With worsening PAD, patients start to develop leg ulcers (open wounds or sores) which fail to heal spontaneously. Some patients develop recurrent infections in the legs with reddening or blackening of the skin. (Critical limb ischemia)


3. What are the causes (risk factors) for PAD?
There are multiple factors which contribute to the development of PAD.
- Diabetes
- Smoking
- Hypertension (High BP)
- Increased blood cholesterol
- Obesity
- Kidney disease (‘Chronic kidney disease’)
- Family history
4. How is PAD diagnosed? What are the routinely performed investigations ?
The diagnosis of PAD is suspected based on the clinical history and physical examination.
The diagnosis is confirmed by the following tests
- Ankle-brachial index – The test is done by to compare the blood pressure in your arm and at the level of the ankle. The test is done by tying a BP cuff to your arm and the ankle, and by using doppler.
- Vascular Ultrasound (Colour doppler study) – The test is done using an Ultrasound machine by placing a hand-held probe on the legs to assess the arteries.
- CT angiography – This test is a CT scan done by injecting the dye (contrast) through the vein to assess the status of the leg arteries.
- Catheter angiography (Digital subtraction angiography, DSA) – This is an invasive test done by injecting ‘contrast’ (iodine-based contrast is the dye which highlights the blood vessels) directly into the blood vessels supplying the legs. This is achieved by passing a thin tube called a ‘catheter’ through the upper thigh or through the wrist and advancing it into the arteries supplying the affected leg . The procedure typically lasts around 20 minutes and is performed under local anaesthesia.
- Carbon dioxide angiography (CO2 angiography) – This angiography is done by substituting Carbon dioxide for iodine-based contrast when performing Catheter angiography. This technique is useful in patients with kidney disease or allergy to iodine-based contrast.
5. How is PAD treated?
The following are the measures used in the treatment of PAD.
- Lifestyle changes – See Q & A 8 below
- Medications
- Anti-platelet medications (Eg. Aspirin, Clopidogrel)
- Lipid-lowering drugs (“Statins”)
- Drugs to reduce the claudication pain – (Cilostazol)
- Exercise programs – Exercise programs help in patients with intermittent claudication. They help in development of collateral pathways (natural bypass channels for blood flow). They can be performed for 30 – 45 minutes in a day, three times a week. The patient can start walking and stop when he feels moderate claudication; and again restart once the pain subsides. This Start/stop cycle can be continued for the duration of exercise. Consult your doctor if you intend to start an exercise program.
- Procedures to restore blood flow (Surgical or Interventional)
- Surgical bypass techniques – This procedure is similar to a bypass surgery done in the heart. It is done by placing a bypass channel (made of synthetic graft; or a vein taken from another body location) so that blood bypasses the occluded blood vessel.
- Interventional techniques – These are minimally invasive procedures done through small nicks. The procedures involve advancing small wires and tubes (catheters) through tiny incisions to open the occluded vessels. Subsequently, the occluded segments are kept open by inflating balloons or by placing stents.
The treating physician will be assessing your clinical condition and the angiogram images to determine which treatment would be appropriate for the patient.



6. When is Angioplasty/Stenting or Bypass surgery needed?
Not all patients with PAD will need procedures to improve the blood flow. Patients with milder forms of claudication can be treated without procedures (Bypass surgery or Angioplasty/Stenting). These procedures are indicated only when the patient has these problems.
- Claudication pain that is limiting patient’s daily routine
- Rest pain
- Non-healing ulcers
- Repeated infections in the legs
7. What are the other medical problems that a PAD patient is likely to encounter?
Atherosclerosis, which is the cause for PAD, can occur in other blood vessels of the human body as well. So PAD patients are at risk of developing other problems like
- Heart attack – disease affecting the ‘coronary’ arteries (arteries supplying the heart muscle)
- Stroke – Disease affecting the carotid arteries and/or other brain-supplying arteries
- Atherosclerosis can also affect other arteries, rarely, like Renal arteries (to the kidneys), mesenteric arteries (to the intestines).
8. How can PAD be prevented? What are the lifestyle changes to prevent Atherosclerosis and its associated diseases?



Lifestyle changes are crucial in preventing (and also treating) Peripheral vascular disease. These lifestyle changes are also appropriate for all diseases caused by ‘Atherosclerosis’ (including Carotid artery disease, Abdominal aortic aneurysm, Coronary artery disease)
- Healthy and nutritious diet – rich in fruits and vegetables, antioxidants.
- Avoiding fat and cholesterol
- Regular exercise
- Maintaining a healthy body weight
- Avoiding smoking
- Proper treatment of chronic ailments (like Hypertension, diabetes and elevated blood cholesterol)